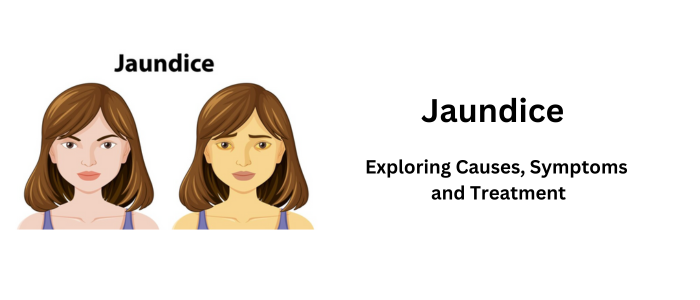
Jaundice: Exploring Causes, Symptoms, and Treatment – Jaundice is a condition in which the skin, whites of the eyes, and mucous membranes turn yellow. This is caused by a buildup of bilirubin in the blood. Bilirubin is a yellow waste product that is produced when red blood cells break down. It is normally processed by the liver and excreted in the bile, which is a digestive fluid. However, if the liver is not functioning properly or the bile ducts are blocked, bilirubin can build up in the blood and cause jaundice.
Table of Contents
What is Jaundice?
Jaundice, also known as icterus, is a medical condition characterized by the yellowing of the skin, eyes, and mucous membranes. This yellowing occurs when there is an excessive buildup of bilirubin in the body. Bilirubin is a yellow pigment produced during the breakdown of red blood cells and is typically processed and excreted by the liver. When this process is disrupted, bilirubin accumulates, leading to the characteristic yellow discoloration.
Causes of Jaundice
Jaundice is not a disease itself but a symptom of an underlying medical condition. It is characterized by a yellowing of the skin, whites of the eyes, and mucous membranes due to an excess of bilirubin in the blood. Bilirubin is a yellow pigment that is produced when red blood cells break down. There are several potential causes of jaundice:
1. Hepatitis:
Hepatitis is a viral infection causing liver inflammation. There are several types, including Hepatitis A, B, C, D, and E, each transmitted differently. Symptoms range from mild to severe and can include jaundice, fatigue, abdominal pain, and nausea. Hepatitis A and B have vaccines, while Hepatitis C is curable with antiviral medication. Chronic Hepatitis B and C can lead to severe complications, including liver cirrhosis and cancer, making early detection crucial.
2. Liver diseases:
Various illnesses that have an impact on the structure and operation of the liver are referred to as liver diseases. Numerous factors, such as alcohol misuse, viral infections (such as hepatitis), obesity, hereditary factors, and more can contribute to the development of these disorders. Cirrhosis, fatty liver disease, alcoholic liver disease, and viral hepatitis are examples of common liver illnesses. Jaundice, exhaustion, stomach pain, and liver malfunction are possible symptoms. It’s crucial to diagnose and treat problems as soon as they arise to stop further damage and complications.
3. Hemolytic Anemia:
Red blood cells are rapidly destroyed in a set of blood illnesses known as hemolytic anemia, which results in a deficiency of these cells in the bloodstream. It may be brought on by a number of things, such as inherited genetic disorders, autoimmune reactions, infections, drugs, or underlying medical diseases. Fatigue, jaundice (caused by the release of bilirubin from damaged red blood cells), and paleness are common symptoms. Depending on the underlying reason, treatment options may include blood transfusions, medicines, or, in extreme circumstances, surgical procedures.
4. Liver Cirrhosis:
Liver cirrhosis is an advanced and irreversible scarring of the liver tissue, often resulting from long-term liver damage and inflammation. It can be caused by chronic alcohol abuse, viral hepatitis (especially Hepatitis B and C), fatty liver disease, or other conditions. As cirrhosis progresses, the liver’s function deteriorates, leading to symptoms like jaundice, fluid retention, fatigue, and confusion. Early diagnosis and lifestyle changes, such as alcohol cessation, can help manage cirrhosis, but advanced cases may require a liver transplant for survival.
5. Obstruction of bile ducts:
Obstruction of the bile ducts refers to a blockage or narrowing of the tubes (ducts) that carry bile from the liver and gallbladder to the small intestine. This obstruction can occur due to various reasons, including:
1. Gallstones:
Small, hardened deposits that can block the common bile duct or the ducts within the gallbladder itself.
2. Tumors:
Both benign and malignant tumors in the liver, gallbladder, or pancreas can compress or invade the bile ducts.
3. Pancreatitis:
Pancreatitis is pancreas inflammation. It can be acute or chronic, often caused by gallstones or excessive alcohol use. Symptoms include severe abdominal pain, nausea, and vomiting. Treatment varies based on the cause and may require hospitalization and dietary changes.
4. Medications:
Some medications can lead to pancreatitis as a side effect.
6. Newborn Jaundice:
Infants frequently suffer from newborn jaundice, also referred to as neonatal jaundice, which is characterized by yellowing of the skin and eyes. It happens because the baby’s blood contains too much of the yellow pigment bilirubin. As a result of their undeveloped liver function, newborns frequently have trouble metabolizing bilirubin. Mild jaundice is typically harmless and goes away on its own. To lower bilirubin levels and avoid consequences, severe jaundice may need treatment, such as phototherapy or exchange transfusion. Parents should keep an eye on their child’s jaundice and seek medical advice if it persists or gets worse.
Symptoms of Jaundice
Jaundice is a condition characterized by the yellowing of the skin, whites of the eyes, and mucous membranes due to elevated levels of bilirubin in the blood. Symptoms of jaundice can vary depending on the underlying cause and the severity of the condition. Common symptoms and signs of jaundice may include:
- Dark urine.
- Pale stools.
- Fatigue and weakness.
- Abdominal pain and discomfort.
- Itchy skin.
- Nausea and vomiting.
- Yellow Skin and Eye
- Loss of Appetites
Types of Jaundice
Jaundice is not a single condition but rather a symptom of an underlying medical issue. It can be categorized into different types based on the cause and the mechanisms involved. The three main types of jaundice are:
1. Pre-hepatic Jaundice (Hemolytic Jaundice):
This kind of jaundice is generally brought on by an excessive breakdown of red blood cells, which results in a rise in bilirubin production. Hemolytic anemias, such as sickle cell anemia, thalassemia, or hereditary spherocytosis, can cause pre-hepatic jaundice.
2. Hepatic Jaundice (Hepatocellular Jaundice):
When the liver is unable to properly process bilirubin due to an internal issue, hepatic jaundice develops. Hepatic jaundice can be caused by a number of liver conditions, including cirrhosis, alcoholic liver disease, hepatitis, and several drugs.
3. Post-hepatic Jaundice (Obstructive Jaundice):
A bile duct obstruction that prevents bilirubin from being discharged into the small intestine is the cause of post-hepatic jaundice. Gallstones, tumors, or bile duct inflammation are common causes of post-hepatic jaundice, as well as illnesses like pancreatic cancer or parasites.
Prevention of Jaundice
The prevention of jaundice largely depends on the underlying causes, as jaundice itself is a symptom of an underlying medical condition rather than a disease that can be directly prevented. However, there are measures you can take to reduce the risk of certain conditions that may lead to jaundice. Here are some preventive strategies:
- Getting vaccinated against hepatitis A and B.
- Drinking alcohol in moderation or abstaining.
- Practicing safe sex to reduce the risk of hepatitis transmission.
- Eating a balanced diet and maintaining a healthy lifestyle.
Diagnosis of Jaundice
The diagnosis of jaundice involves a series of medical evaluations and tests to determine the underlying cause of the condition. Here are the key steps in diagnosing jaundice:
Medical History and Physical Examination
Blood Tests
Imaging Studies
Endoscopic Procedures
Liver Biopsy
Stool Color and Urine Color
Medical History
Treatment of Jaundice
The treatment for jaundice depends on its underlying cause. Here are some common treatment approaches:
1. Managing Underlying Conditions:
Effective management of underlying medical conditions involves regular medical consultations, adherence to prescribed medications, lifestyle adjustments like diet and exercise, self-monitoring, stress reduction, and support networks. Monitoring and early intervention through routine check-ups, adherence to medical advice, and maintaining a medication schedule are key to successfully managing chronic illnesses while ensuring a better quality of life.
2. Liver Transplant:
A liver transplant is a surgical procedure in which a damaged or diseased liver is replaced with a healthy liver from a deceased or living donor. It is typically considered for individuals with end-stage liver disease, acute liver failure, or specific liver cancers. The procedure offers a chance for a longer and healthier life. However, it is a complex surgery that requires careful evaluation, extensive recovery, and lifelong medical management to prevent rejection and complications.
3. Medication:
Medications, also known as drugs or pharmaceuticals, are substances used to diagnose, treat, cure, or prevent diseases. They can be prescribed by healthcare professionals or purchased over-the-counter. Medications work in various ways, targeting specific biological pathways or symptoms. It’s crucial to follow prescribed dosages and instructions to ensure effectiveness and safety. Side effects and interactions can occur, so communication with healthcare providers is essential for proper medication management and overall well-being.
4. Lifestyle Changes:
Lifestyle changes encompass adjustments in daily habits for improved well-being. A balanced diet with whole foods, regular physical activity, and weight management reduce the risk of chronic diseases. Smoking cessation is vital for lung and heart health, while moderate alcohol consumption supports overall well-being. Stress management techniques like meditation promote mental health, and adequate sleep is essential. Staying hydrated, taking medications as prescribed, and regular medical check-ups ensure a healthy, fulfilling life. Customized lifestyle changes can greatly impact an individual’s health and long-term quality of life.
Conclusion
Jaundice is a medical condition characterized by yellowing of the skin and eyes, often caused by the buildup of bilirubin in the body. It can have various underlying causes, ranging from liver diseases to genetic conditions. Prompt diagnosis and appropriate treatment are essential to manage jaundice effectively. If you or someone you know is experiencing symptoms of jaundice, it’s crucial to seek medical advice for a proper evaluation and care.

